Dr. Mercola recently posted on his website regarding the health risks he sees in root canals. Mind you, the emphasis isn’t on root canals themselves, because Dr. Mercola acknowledges that root canals save teeth. His concern is more with whole-body health. He cites the research of a 20th-Century dentist Dr. Weston Price (and more contemporary research as well) to show a strong correlation between root canals and a range of chronic, inflammatory diseases and cancers. More specifically, these diseases range from heart, kidney, joint, neurological and autoimmune diseases to breast cancer. The culprit in many cases is explained as toxins produced by bacteria entombed in the tooth and in the tissues surrounding the tooth. These toxins can then inhibit and sometimes “short-circuit” the immune system, resulting in either too much, not enough, or mis-applied inflammation.
The Crux: Disinfection
What? Bacteria entombed in the tooth?
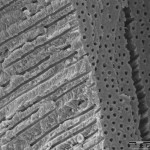
Dentists are taught to do root canals by soaking the canals in good ol’e fashioned bleach. The idea is that this disinfects the tooth, so that even though it’s “dead” (no blood supply nor nerves inside it), it’s not technically decayed anymore. Mainstream dentistry teaches that once the tooth’s disinfected it can be filled with a sealing material and then crowned for strength. The critique from the other side of the fence has to do with the structure of the tooth and fluid dynamics. The argument goes like this: Teeth frequently have extra “tributary” and connecting channels that run between and off of the main canals. It’s difficult to fully clean all the infected tissue from these auxilliary canals simply because they can’t be reached with an instrument. Similarly, Dentin — the stuff to be disinfected — is extremely porous with little tubules running from inside to outside, with connections between tubles too (envision a cross-section of pine under a microscope). Critics ask: When these canals and microtubles are already filled with fluid, how can disinfectant fully penetrate them all the way out to the cementum? And even if you do fully disinfect the tooth, how can those tubules stay disinfected given that some of them end above the gums and that there are connections between them?
The Other Side: But It’s My Tooth!
The American Dental Association and a great many endodontic organizations maintain that root canals are successful– and millions of asymptomatic teeth are the evidence. And when you have a dentist telling you that it’s either a root canal or an extraction, the evidence for root canals sounds pretty darn good.
And there are many situations in which disinfection seems more likely: not all infected teeth are “dirty” all the way out the end of the root. If the decay is already into the pulp but barely so, the immune system may have prevented the infection from even getting down into the canals. In these situations a root canal or other even more conservative options seem to serve both sides of the issue.
Other Root Canal Treatment Options
If you’d rather not have a root canal, there are alternatives. After extraction, you can:
1: restore the tooth with an implant
2: restore the tooth with a bridge
3: restore the tooth with a removable tooth (a denture)
or
4: leave the tooth unrestored. Sometimes this can affect your bite if teeth move afterward.
Implants can be made of titanium or zirconium. There are pros and cons to each. Traditional dentistry tends to favor titanium because of its longer track record and familiarity. It also has a very low percentage of patients being sensitive to it. In some cases, zirconium can darken the gums in esthetic areas. Also, some critics of titanium don’t like the idea of any metal in the mouth. If increased esthetics or non-metallic implants are your preference, zirconium implants may be your preferred option.
Zirconium implants are newer (recently FDA approved but with a longer track record in Europe), highly esthetic (they’re white like a tooth), and hold great promise for those who prefer a metal-free mouth. The cons (compared to titanium): During the healing period after placement, zirconium implants require more protection in the mouth that titanium implants do. They’re also more brittle than titanium, requiring them to be “one-piece: a monolithic implant which the crown is placed directly on. Titanium implants, on the other hand, can accept all kinds of fittings and hardware due to their internal threads. However, plenty of clincial evidence shows that once they’re properly-protected during healing, one-piece zirconium implants do work and work well.
A bridge restores the tooth by attaching the crown to crowns on the two adjacent teeth. This option was considered the standard of care before implants. Its disadvantages are that it is less conservative for the adjacent teeth, that cleaning is more difficult (you have to clean under the bridge), and that if the bridge gets decay under it, the entire bridge needs to be replaced. Its advantages are that it’s non-surgical and that initially it costs a little less than an implant restoration.
A removable tooth (denture) is a plastic or metal-and-plastic replacement for one or more teeth. These are less expensive but also much less functional than an implant or bridge.
In the End
Whether you decide on a root canal, an implant, a bridge or a denture, it’s a decision that only you can make the decision on restoring your infected tooth.
Here is Dr. Mercola’s Report. You can also view it in full on his website.
Do you have a chronic degenerative disease? If so, have you been told, “It’s all in your head?”
Well, that might not be that far from the truth… the root cause of your illness may be in your mouth.
There is a common dental procedure that nearly every dentist will tell you is completely safe, despite the fact that scientists have been warning of its dangers for more than 100 years.
Every day in the United States alone, 41,000 of these dental procedures are performed on patients who believe they are safely and permanently fixing their problem.
What is this dental procedure?
The root canal.
More than 25 million root canals are performed every year in this country.
Root-canaled teeth are essentially “dead” teeth that can become silent incubators for highly toxic anaerobic bacteria that can, under certain conditions, make their way into your bloodstream to cause a number of serious medical conditions—many not appearing until decades later.
Most of these toxic teeth feel and look fine for many years, which make their role in systemic disease even harder to trace back.
Sadly, the vast majority of dentists are oblivious to the serious potential health risks they are exposing their patients to, risks that persist for the rest of their patients’ lives.The American Dental Association claims root canals have been proven safe, but they have NO published data or actual research to substantiate this claim.
Fortunately, I had some early mentors like Dr. Tom Stone and Dr. Douglas Cook, who educated me on this issue nearly 20 years ago. Were it not for a brilliant pioneering dentist who, more than a century ago, made the connection between root-canaled teeth and disease, this underlying cause of disease may have remained hidden to this day. The dentist’s name was Weston Price—regarded by many as the greatest dentist of all time.
Weston A. Price: World’s Greatest Dentist
Most dentists would be doing an enormous service to public health if they familiarized themselves with the work of Dr. Weston Pricei. Unfortunately, his work continues to be discounted and suppressed by medical and dental professionals alike.
Dr. Price was a dentist and researcher who traveled the world to study the teeth, bones, and diets of native populations living without the “benefit” of modern food. Around the year 1900, Price had been treating persistent root canal infections and became suspicious that root-canaled teeth always remained infected, in spite of treatments. Then one day, he recommended to a woman, wheelchair bound for six years, to have her root canal tooth extracted, even though it appeared to be fine.
She agreed, so he extracted her tooth and then implanted it under the skin of a rabbit. The rabbit amazingly developed the same crippling arthritis as the woman and died from the infection 10 days later. But the woman, now free of the toxic tooth, immediately recovered from her arthritis and could now walk without even the assistance of a cane.
Price discovered that it’s mechanically impossible to sterilize a root-canaled (e.g. root-filled) tooth.
He then went on to show that many chronic degenerative diseases originate from root-filled teeth—the most frequent being heart and circulatory diseases. He actually found 16 different causative bacterial agents for these conditions. But there were also strong correlations between root-filled teeth and diseases of the joints, brain and nervous system. Dr. Price went on to write two groundbreaking books in 1922 detailing his research into the link between dental pathology and chronic illness. Unfortunately, his work was deliberately buried for 70 years, until finally one endodontist named George Meinig recognized the importance of Price’s work and sought to expose the truth.
Dr. Meinig Advances the Work of Dr. Price
Dr. Meinig, a native of Chicago, was a captain in the U.S. Army during World War II before moving to Hollywood to become a dentist for the stars. He eventually became one of the founding members of the American Association of Endodontists (root canal specialists).
In the 1990s, he spent 18 months immersed in Dr. Price’s research. In June of 1993, Dr. Meinig published the book Root Canal Cover-Up, which continues to be the most comprehensive reference on this topic today. You can order your copy directly from the Price-Pottenger Foundationii.
What Dentists Don’t Know About the Anatomy of Your Teeth
Your teeth are made of the hardest substances in your body.
In the middle of each tooth is the pulp chamber, a soft living inner structure that houses blood vessels and nerves. Surrounding the pulp chamber is the dentin, which is made of living cells that secrete a hard mineral substance. The outermost and hardest layer of your tooth is the white enamel, which encases the dentin.
The roots of each tooth descend into your jawbone and are held in place by the periodontal ligament. In dental school, dentists are taught that each tooth has one to four major canals. However, there are accessory canals that are never mentioned. Literally miles of them!
Just as your body has large blood vessels that branch down into very small capillaries, each of your teeth has a maze of very tiny tubules that, if stretched out, would extend for three miles. Weston Price identified as many as 75 separate accessory canals in a single central incisor (front tooth). For a more detailed explanation, refer to an article by Hal Huggins, DDS, MS, on the Weston A. Price Foundation website.iii(These images are borrowed from the Huggins article.)
Microscopic organisms regularly move in and around these tubules, like gophers in underground tunnels.
When a dentist performs a root canal, he or she hollows out the tooth, then fills the hollow chamber with a substance (called guttapercha), which cuts off the tooth from its blood supply, so fluid can no longer circulate through the tooth. But the maze of tiny tubules remains. And bacteria, cut off from their food supply, hide out in these tunnels where they are remarkably safe from antibiotics and your own body’s immune defenses.
The Root Cause of Much Disease
Under the stresses of oxygen and nutrient deprivation, these formerly friendly organisms morph into stronger, more virulent anaerobes that produce a variety of potent toxins. What were once ordinary, friendly oral bacteria mutate into highly toxic pathogens lurking in the tubules of the dead tooth, just awaiting an opportunity to spread.
No amount of sterilization has been found effective in reaching these tubules—and just about every single root-canaled tooth has been found colonized by these bacteria, especially around the apex and in the periodontal ligament. Oftentimes, the infection extends down into the jawbone where it creates cavitations—areas of necrotic tissue in the jawbone itself.
Cavitations are areas of unhealed bone, often accompanied by pockets of infected tissue and gangrene. Sometimes they form after a tooth extraction (such as a wisdom tooth extraction), but they can also follow a root canal. According to Weston Price Foundation, in the records of 5,000 surgical cavitation cleanings, only two were found healed.
And all of this occurs with few, if any, accompanying symptoms. So you may have an abscessed dead tooth and not know it. This focal infection in the immediate area of the root-canaled tooth is bad enough, but the damage doesn’t stop there.
Root Canals Can Lead to Heart, Kidney, Bone, and Brain Disease
As long as your immune system remains strong, any bacteria that stray away from the infected tooth are captured and destroyed. But once your immune system is weakened by something like an accident or illness or other trauma, your immune system may be unable to keep the infection in check.
These bacteria can migrate out into surrounding tissues by hitching a ride into your blood stream, where they are transported to new locations to set up camp. The new location can be any organ or gland or tissue.
Dr. Price was able to transfer diseases harbored by humans to rabbits, by implanting fragments of root-canaled teeth, as mentioned above. He found that root canal fragments from a person who had suffered a heart attack, when implanted into a rabbit, would cause a heart attack in the rabbit within a few weeks.
He discovered he could transfer heart disease to the rabbit 100 percent of the time! Other diseases were more than 80 percent transferable by this method. Nearly every chronic degenerative disease has been linked with root canals, including:
- Heart disease
- Kidney disease
- Arthritis, joint, and rheumatic diseases
- Neurological diseases (including ALS and MS)
- Autoimmune diseases (Lupus and more)
There may also be a cancer connection. Dr. Robert Jones, a researcher of therelationship between root canals and breast cancer, found an extremely high correlation between root canals and breast cancer.iv He claims to have found the following correlations in a five-year study of 300 breast cancer cases:
- 93 percent of women with breast cancer had root canals
- 7 percent had other oral pathology
- Tumors, in the majority of cases, occurred on the same side of the body as the root canal(s) or other oral pathology
Dr. Jones claims that toxins from the bacteria in an infected tooth or jawbone are able to inhibit the proteins that suppress tumor development. A German physician reported similar findings. Dr. Josef Issels reported that, in his 40 years of treating “terminal” cancer patients, 97 percent of his cancer patients had root canals. If these physicians are correct, the cure for cancer may be as simple as having a tooth pulled, then rebuilding your immune system.
Good Bugs Gone Bad
How are these mutant oral bacteria connected with heart disease or arthritis? The ADA and the AAE claim it’s a “myth” that the bacteria found in and around root-canaled teeth can cause diseasev. But they base that on the misguided assumption that the bacteria in these diseased teeth are the SAME as normal bacteria in your mouth—and that’s clearly not the case.
Today, bacteria can be identified using DNA analysis, whether they’re dead or alive, from their telltale DNA signatures.
In a continuation of Dr. Price’s work, the Toxic Element Research Foundation (TERF) used DNA analysis to examine root-canaled teeth, and they found bacterial contamination in 100 percent of the samples tested. They identified 42 different species of anaerobic bacteria in 43 root canal samples. In cavitations, 67 different bacteria were identified among the 85 samples tested, with individual samples housing between 19 to 53 types of bacteria each. The bacteria they found included the following types:
- Capnocytophagaochraceavi
- Fusobacteriumnucleatumvii
- Gemellamorbillorum viii
- Leptotrichiabuccalis
- Porphyromonasgingivalis ix
Are these just benign, ordinary mouth bugs? Absolutely not. Four can affect your heart, three can affect your nerves, two can affect your kidneys, two can affect your brain, and one can infect your sinus cavities… so they are anything BUT friendly! (If you want see just how unfriendly they can be, I invite you to investigate the footnotes.)
Approximately 400 percent more bacteria were found in the blood surrounding the root canal tooth than were found in the tooth itself, suggesting the tooth is the incubatorand the periodontal ligament is the food supply. The bone surrounding root-canaled teeth was found even HIGHER in bacterial count… not surprising, since bone is virtual buffet of bacterial nutrients.
Since When is Leaving A Dead Body Part IN Your Body a Good Idea?
There is no other medical procedure that involves allowing a dead body part to remain in your body. When your appendix dies, it’s removed. If you get frostbite or gangrene on a finger or toe, it is amputated. If a baby dies in utero, the body typically initiates a miscarriage.
Your immune system doesn’t care for dead substances, and just the presence of dead tissue can cause your system to launch an attack, which is another reason to avoid root canals—they leave behind a dead tooth.
Infection, plus the autoimmune rejection reaction, causes more bacteria to collect around the dead tissue. In the case of a root canal, bacteria are given the opportunity to flush into your blood stream every time you bite down.
Why Dentists Cling to the Belief Root Canals are Safe
The ADA rejects Dr. Price’s evidence, claiming root canals are safe, yet they offer no published data or actual research to substantiate their claim. American Heart Association recommends a dose of antibiotics before many routine dental procedures to prevent infective endocarditis (IE) if you have certain heart conditions that predispose you to this type of infection.
So, on the one hand, the ADA acknowledges oral bacteria can make their way from your mouth to your heart and cause a life-threatening infection.
But at the same time, the industry vehemently denies any possibility that these same bacteria—toxic strains KNOWN to be pathogenic to humans—can hide out in your dead root-canaled tooth to be released into your blood stream every time you chew, where they can damage your health in a multitude of ways.
Is this really that large of a leap? Could there be another reason so many dentists, as well as the ADA and the AAE, refuse to admit root canals are dangerous? Well, yes, as a matter of fact, there is. Root canals are the most profitable procedure in dentistry.x
What You Need to Know to AVOID a Root Canal
I strongly recommend never getting a root canal. Risking your health to preserve a tooth simply doesn’t make sense. Unfortunately, there are many people who’ve already have one. If you have, you should seriously consider having the tooth removed, even if it looks and feels fine. Remember, as soon as your immune system is compromised, your risk of of developing a serious medical problem increases—and assaults on your immune system are far too frequent in today’s world.
If you have a tooth removed, there are a few options available to you.
- Partial denture: This is a removable denture, often just called a “partial.” It’s the simplest and least expensive option.
- Bridge: This is a more permanent fixture resembling a real tooth but is a bit more involved and expensive to build.
- Implant: This is a permanent artificial tooth, typically titanium, implanted in your gums and jaw. There are some problems with these due to reactions to the metals used. Zirconium is a newer implant material that shows promise for fewer complications.
But just pulling the tooth and inserting some sort of artificial replacement isn’t enough.
Dentists are taught to remove the tooth but leave your periodontal ligament. But as you now know, this ligament can serve as a breeding ground for deadly bacteria. Most experts who’ve studied this recommend removing the ligament, along with one millimeter of the bony socket, in order to drastically reduce your risk of developing an infection from the bacterially infected tissues left behind.
I strongly recommend consulting a biological dentist because they are uniquely trained to do these extractions properly and safely, as well as being adept at removing mercury fillings, if necessary. Their approach to dental care is far more holistic and considers the impact on your entire body—not JUST your mouth.
If you need to find a biological dentist in your area, I recommend visiting toxicteeth.orgxi, a resource sponsored by Consumers for Dental Choice. This organization, championed by Charlie Brown, is a highly reputable organization that has fought to protect and educate consumers so that they can make better-informed decisions about their dental care. The organization also heads up the Campaign for Mercury-Free Dentistry.